Introduction
Transrectal ultrasound-guided prostate biopsy (TRUS-Bx) is considered the current diagnostic standard for patients with suspected prostate cancer (PCa) based on raised serum prostatic specific antigen (PSA) levels, abnormal digital rectal examination findings and other risk factors.
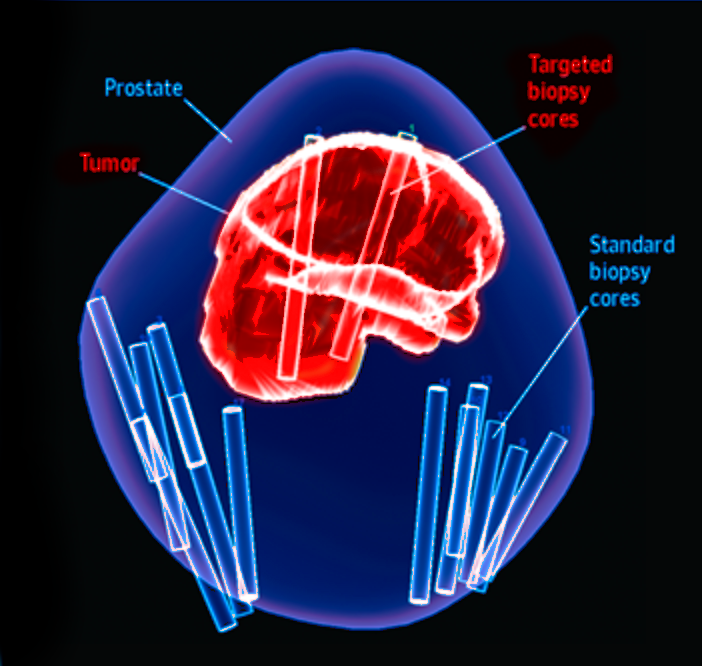
Recent years have seen significant advances in magnetic resonance imaging (MRI) technology. Increasing evidence suggests that MRI could non-invasively improve PCa visualization and aid in targeting prostate biopsies to abnormal areas seen on MRI. Hence, an approach with a pre-biopsy MRI followed by targeted biopsy (TBx), namely the “MRI pathway”, has become feasible, and studies have shown that MRI-targeted biopsy may improve detection of PCa.